Abstract
Introduction: About one third of patients with diffuse large B-cell lymphoma (DLBCL) fail frontline treatment or have early relapse. Baseline quantitative parameters derived from positron emission computed tomography (PET/CT) at baseline may predict outcome in DLBCL patients. However, their prognostic value in interim scans is unclear. Recently, the role delta maximum standardized uptake value (ΔSUVmax) has been tested as a predictor of PFS. In this retrospective study we aimed to analyze the role of ΔSUVmax between baseline and interim PET-CT as a predictor of progression of disease within 1 year in DLBCL patients and, to compare this parameter to the standard validated method to evaluate disease response: Deauville scale (DS).
Methods: This is a single-center retrospective cohort study from São Paulo, Brazil. We included patients with DLBCL who had baseline (b-PET) and interim (i-PET, after 2-3 cycles of treatment) PET-CTs and who have been treated with 6 cycles of R-CHOP given every 21 days. All PET-CTs were analyzed by the same physician and blinded for the clinical features. Delta maximum standardized uptake value (ΔSUVmax) was calculated by the difference in % between initial PET SUVmax and iPET SUVmax. The objective was to assess if ΔSUV performed better than Deauville scale (DS) in predicting early disease progression. Cut-off values were defined by receiver operating characteristic (ROC) analysis. Analysis was performed with Cox model. Model comparison was based on the lowest AIC.
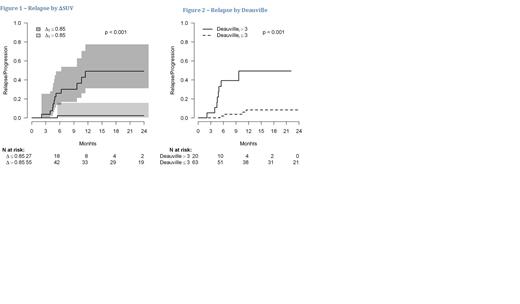
Results: A total of 83 patients with DLBCL were available for analyses. The median age was 60 years and 66% of patients had a germinal center B-Cell (GCB) phenotype. With median follow-up of 15 months, patients with a cut-off ΔSUVmax <85% had a higher risk of disease relapse (49% vs 2%, p<0.001) at 12 months (figure 1). Patients with DS >3 in the iPET were also at a higher risk of disease progression (p<0.001) (figure 2). The model with ΔSUVmax was better adjusted (AIC=86) than the one with DS (AIC=92). The median maximum uptake at baseline PET/CT, MYC and/or BCl2 expression were not predictive of relapse at 12 months. International prognostic index (IPI) was also predictive of relapse (p=0.003), but again performed poorer than ΔSUVmax (AIC=99).
Discussion/Conclusion: We showed that ΔSUVmax quantitative PET-CT model has superior discriminatory power than the qualitative DS model and the clinical IPI. Although we have a small sample, this finding corresponds with PETAL trial, which also showed that the ΔSUVmax method is superior to the commonly used Deauville five-point scale to identify patients at high risk of treatment fails. Although, the ΔSUVmax cut-off value calculated in our study was 85%, while in the PETAL study a reduction off 66% in the baseline SUV was the considered cutoff. Maybe, combing ΔSUVmax method in a with DS and IPI can improve prognostic stratification and early identification of high risk DLBCL. The ΔSUVmax is an easily reproducible method, that can be easily assessed by PET-CT, differing from other quantitative measures like the total metabolic tumor volume. In conclusion, further validation in a large sample of patients should be performed before the incorporation of quantitative PET-CT methods in clinical practice however it is a promising prognostic marker.
Perini: Janssen: Honoraria, Speakers Bureau; Takeda: Honoraria, Speakers Bureau; Astra Zeneca: Honoraria, Speakers Bureau; MSD: Honoraria, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal